Your overall chance of success with a first-time IVF cycle depends on many factors, from your hormone levels and uterine lining to your health and fertility history. However, it can also depend on the quality of your embryos and the skill of your clinic.
For example, the grading of your blastocyst embryos can impact ongoing pregnancy rates, as demonstrated by the chart below.
1. Age
A woman’s age has a significant impact on her embryo transfer success rates. The best results are seen in women under 30 years of age, and the rate of implantation decreases as the female patient gets older.
This is due in part to a gradual decline in the quality of the embryos and the uterus’ receptivity to the embryo, which are both affected by the age of the patient. In addition, the rate of aneuploidy (missing chromosomes) increases with age.
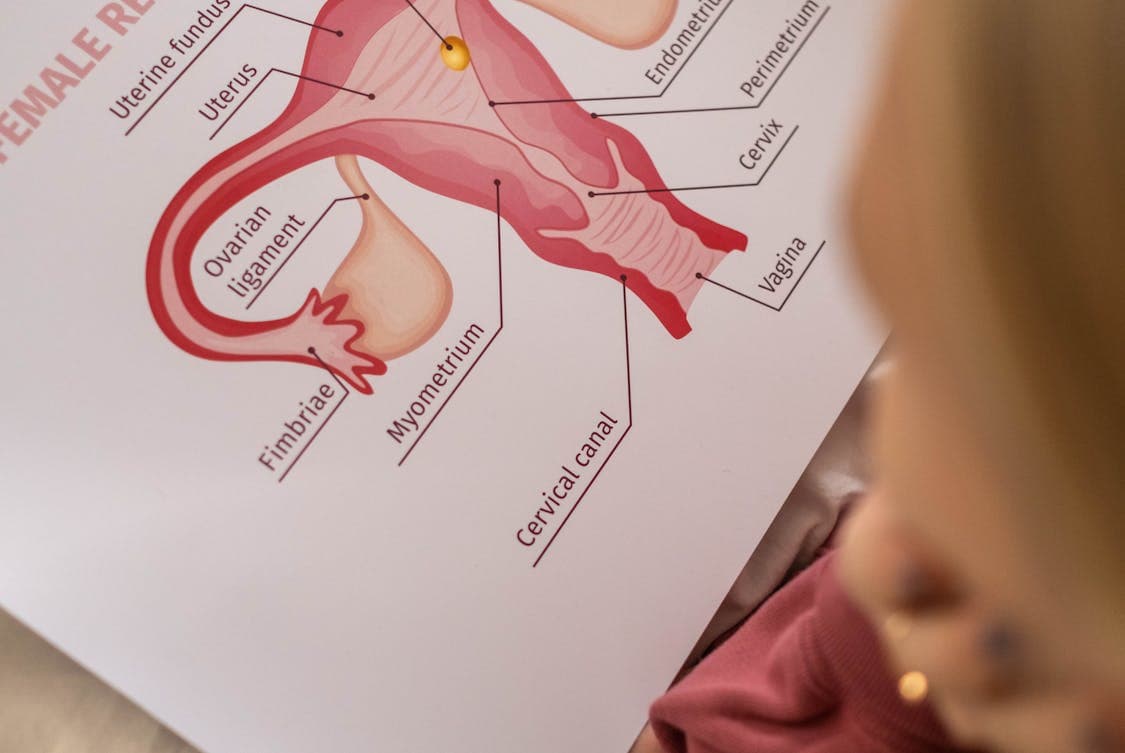
The endometrial lining is important for implantation, and the thickness of this lining can influence the chances of an embryo implanting successfully. The thickness of the lining can be measured by endometrial biopsy. This procedure involves removing a small amount of tissue from the uterus, which can then be tested for receptivity to embryos by an embryologist.
Embryo transfer itself is not painful, although patients may feel some discomfort when a speculum or catheter are inserted into the cervix. After the uterus is prepared, the doctor will load the euploid embryo into the transfer catheter and position it in the uterus using ultrasound guidance. The patient will then be allowed to rest. In the following days, follow-up appointments will be scheduled for bloodwork and an ultrasound to check on the status of the lining.
Embryo transfer is not as complicated as it sounds, but there are some things that you should keep in mind in order to improve your odds of success. These include avoiding hot baths and saunas, limiting stress, and abstaining from intercourse until your doctor says it’s safe to do so. It is also crucial to continue taking your prescribed medications, such as progesterone, which helps to support the lining of the uterus.
2. Embryo Quality
When a fertilized egg starts developing, it goes through several stages and the quality of these embryos is crucial to the success of assisted reproductive technologies like in vitro fertilisation (IVF) and surrogacy. Embryos are graded and assessed for their quality after fertilization by highly trained embryologists based on a number of parameters. The grading process is meticulous and takes into account the cleavage phase, kinetics of cell division, the number, symmetry and spatial arrangement of blastomeres on days 2 and 3, the absence or presence of multinucleation, the cellular compaction, granularity and thickness of the zona pellucida (ZP).
Eventually the embryo will reach the blastocyst stage. A blastocyst consists of two different groups of cells; the inner cell mass (ICM) which forms the fetus and the trophectoderm (TE) that forms the placenta. Both groups of cells are graded based on their morphology. An embryo with excellent morphology has tightly packed and well-defined cells which indicates a higher potential for successful implantation and fetal development. Similarly, an embryo with poor morphology has loose and less defined cells that indicate a lower potential for successful implantation and fetal developments.
Once an embryo has reached the blastocyst stage, it is then referred to as a “top quality” embryo. Top quality means an embryo with no multinucleated blastomeres and a minimum of four blastomeres on day two or seven or more blastomeres on day three. Embryos with high cleavage, cellular compaction and ZP quality are also considered to be of good quality.
The pregnancy rate following a top quality blastocyst transfer is significantly greater than that of a poor-quality one. However, it is important to note that embryo grading alone does not fully predict clinical pregnancy or live birth rates as there are other factors that influence these outcomes such as endometrial receptivity and how well the uterus communicates with the embryo.
3. Ovarian Reserve
Women begin to lose their ovarian reserve as they age, and this diminishes the quality of her eggs. Women with diminished ovarian reserve have lower success rates when trying to conceive with in vitro fertilization (IVF) than women of normal ovarian reserve.
In most cases, aging causes the decline in ovarian reserve. However, genetic defects, aggressive medical treatments that harm the reproductive system (radiation for cancer), and some surgeries can also contribute to diminished ovarian reserve.
Blood tests can be used to measure a woman’s anti-mullerian hormone (AMH) and follicle stimulating hormone (FSH). These levels reflect the amount of potential eggs in her ovaries. A low AMH or a high day 2 or 3 FSH level indicates decreased ovarian reserve. A low antral follicle count (AFC) is also indicative of decreased ovarian reserve.
These blood tests allow us to determine the number of viable eggs available for embryo transfer process. If a woman has low ovarian reserves, a double embryo transfer may be recommended to increase her chances of pregnancy.
If a woman has a normal ovarian reserve, an embryo transfer with a single embryo can result in a successful pregnancy. However, if the woman’s ovarian reserve is poor, she may be better off with a frozen embryo transfer (FET).
FET is more successful than fresh embryo transfers in most situations. It gives the body time to recover from the ovarian stimulation drugs used in IVF, creating a more favorable environment for implantation. Moreover, FET is more cost-effective than fresh embryo transfer, and it is safe for most women. However, there are some instances when fresh embryo transfer may be preferable, such as in women with polycystic ovary syndrome or those at risk for Ovarian Hyperstimulation Syndrome (OHSS). In these situations, we recommend that you choose a clinic with experience performing both techniques.
4. Male Fertility
A man’s reproductive system must make healthy sperm, and the woman’s eggs must be fertilized by those sperm in order for a pregnancy to be formed. For this to happen, sperm must be able to travel from the penis to the uterus, where the egg will then implant. This process can be interfered with if the man’s fallopian tubes are blocked, or if his sperm is unhealthy. In men, infertility can be caused by a hormone imbalance, testicular damage, and genetic issues such as Kleinfelter syndrome.
Approximately 12% of male infertility is caused by primary testicular failure, which can be due to injury, radiation or varicocele. It can also be a result of a congenital disease such as Kleinfelter syndrome or a genetic disorder such as Trisomy 18 or Down Syndrome. Treatment options include semen analysis, a procedure where a sample of the man’s semen is examined in the lab to determine the quality and concentration of the sperm. In addition, medications such as clomiphene citrate or tamoxifen may be used to treat hormone imbalances or low sperm motility.
In a study of 370 frozen embryo transfer cycles using euploid blastocysts (euploid embryos are screened for aneuploidies by next generation sequencing), it was found that ongoing pregnancy rates were significantly higher when excellent-quality blastocysts were transferred compared to average- or poor-quality ones. These findings indicate that it is important to have a high-quality, euploid embryo available for transfer.
5. Lifestyle
The lifestyle of the patient plays a crucial role in the success rate of IVF procedures. In order to maximize your chances of getting pregnant, it is recommended that you refrain from smoking and alcohol consumption, as well as maintain a healthy weight, especially before the IVF procedure. A healthy diet can also help your body to absorb the hormones and other drugs that you will need to take during the course of the treatment, thus making them more effective.
The concept of lifestyle is a central research topic in sociology and psychology, and has been analyzed from various perspectives. Some theorists have identified the internal dimension of lifestyle as a personal characteristic, manifested in daily practices and habits that characterize each individual (see, for example, theories by Adler, Rokeach, Weber, and Bourdieu). Others, such as Giddens, have stressed its temporal aspect, arguing that it is a result of the social dynamics of life in definite phases or environments, and may vary according to the different needs of the individual and of the community.
A more recent view of the concept is that it is a collectively organized social phenomenon, characterized by dynamic processes of identification, differentiation, and recognition at a sociocultural level. This interpretation is reflected in the work of scholars such as Georg Simmel, and has been renewed by authors such as Pierre Bourdieu, who developed a model where lifestyles are formed from both static forces at a macro level and dynamic ones at a micro level.
The latter perspective is the one most embraced by critical health psychology, which proposes to understand a healthy lifestyle as an active process of self-realization and synthesis, and not as a series of behavioral choices made on the basis of health-related goals and objectives.




